Written By: Dr. Mohamed Ghanem
Dr. Mohamed Ghanem is a Specialist in the Department of Orthopaedics. He completed his MBBS from Mansoura University in Egypt and his Master's degree in Orthopaedic and Trauma Surgery (MSc) from Benha University also in Egypt. He is a member of the AO TRAUMA Gulf Cooperation Council, the AO SPINE Gulf Cooperation Council and the Egyptian Orthopaedic Association (EOA).
Updated On:January 29, 2025
Read more.

What is a Herniated Disk?
The nucleus, or soft center, of a spinal disk is covered by a stiffer, rubbery outer layer called the annulus. When a piece of the nucleus slides through a tear in the annulus, it ruptures, causing a herniated disk, also known as a slipped disk or a burst disk.
A herniated disk can form anywhere along the spine. Depending on where it occurs, a herniated disk may result in pain, numbness, or weakness in an arm or leg.
Causes of Herniated Disk
Most frequently, cumulative aging-related wear and tear known as disk degeneration leads to disk herniation. The disks grow less elastic and more prone to rupturing with even a slight strain or twist as people age.
Most people struggle to identify the reason behind their ruptured disk. Twisting and turning while lifting can sometimes result in a herniated disk, as can using the back muscles to raise big objects rather than the leg and thigh muscles.
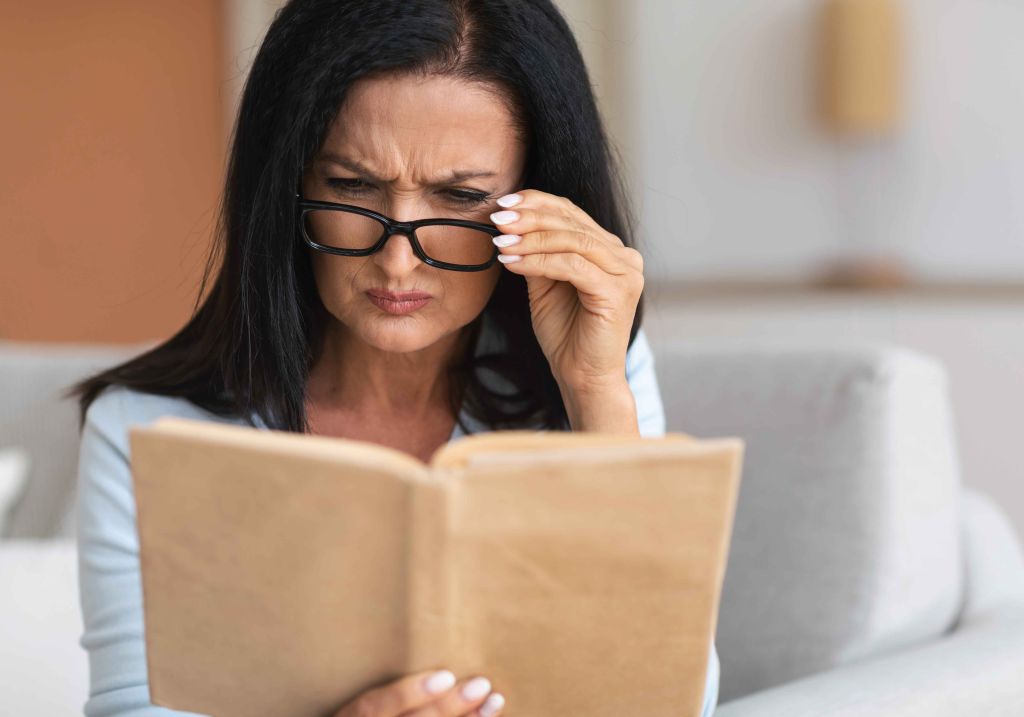
Symptoms of Herniated Disk
Although they can sometimes develop in the neck, herniated disks typically occur in the lower back. The location of the disk and whether it is pressing on a nerve will determine the signs and symptoms. One side of the body is typically affected by herniated disks.
Signs and symptoms of herniated discus include the following:
- In addition to lower back discomfort, you may experience aching in your thighs, calves, and buttocks if your ruptured disk is in your lower back. Your foot can cause you discomfort as well.
- Your shoulder and arm will typically feel the effects of a herniated neck disk the most. When you cough, sneeze, or assume certain positions, your arm or leg can experience pain. Neck herniated disks typically provide piercing or burning discomfort.
- Radiating numbness or tingling in the body area that the injured nerves are supplying is one of the symptoms of a herniated disk.
- Usually, the muscles impacted nerves become weakened. You could struggle to lift things or get unsteady as a result.
A herniated disk might exist without any signs or symptoms. It's possible that you won't be aware of it until a spinal scan reveals it.
When to see a doctor for Herniated Disk?
You need to consult a doctor if you experience any of the following:
- Going to work and other regular activities are hampered by pain
- Symptoms have not improved after four weeks
- Symptoms worsening
- Losing control of bladder and bowels
- Tingling or numbness in arms, hands, legs, or feet
- Loss of strength
- Difficulty walking or standing
Herniated Disk Risk Factors
You are more likely to suffer from a herniated disk due to the following risk factors:
- Weight: When a person is overweight, their lower back disks are impacted.
- Occupation. People who have physically demanding jobs are more prone to have back problems.
- Genetics. Some people are genetically susceptible to developing a herniated disk.
- Smoking. Smoking is believed to decrease the oxygen flow to disks, accelerating their deterioration.
- driving quite a bit. In addition to prolonged sitting, the vibration from a car's engine could strain the spine.
- acting passively. Regular exercise can help you avoid developing a herniated disk.
Herniated Disk Complications
The cauda equina nerves and the entire spinal canal may be compressed by a disk herniation. In rare cases, immediate surgery may be necessary to prevent paralysis or lasting disability.
Get immediate medical help if you have:
- Symptoms getting worse. You may have pain, numbness, or weakness that interferes with your everyday tasks.
- Bowel or bladder problems. Even with a full bladder, cauda equina syndrome can result in incontinence or difficulties urinating.
- Saddle numbing. The inner thighs, the back of the legs, and the region around the rectum are all affected by this increasing loss of sensation.
Herniated Disk Diagnosis
Your doctor will feel any tenderness in your back during the physical examination. To help identify the source of your pain, you might be asked to lay flat and move your legs into various positions.
A neurological examination may also be done by your physician to assess your reflexes, muscle power, ability to walk, and sensations. A physical examination and medical history are typically sufficient for diagnosing herniated disks. One or more of the following tests may be prescribed by your doctor if they suspect another condition or if they need to determine which nerves are impacted.
- Imaging tests
- X-Rays
- CT Scans
- MRIs
- Myelogram
- Nerve tests
- Nerve conduction study
- Electromyography (EMG)
Herniated Disk Treatment
In some cases, herniated disk does not need treatment. However, if your symptoms don't seem to be improving, your healthcare professional might advise one of the following:
- Medication: Your doctor might advise using a muscle relaxant or anti-inflammatory pain reliever.
- Physical therapy: To assist reduce strain on your nerves, a physical therapist offers you an exercise regimen. Exercise helps to increase circulation and relax tense muscles.
- Spinal injections: Also known as an epidural or nerve block, this procedure involves injecting a steroid medicine right into your spine. The drug lessens the nerve's swelling and inflammation caused by the disk herniation. Your body will be able to mend and get back to work more quickly as a result.
- Surgery: Surgery may be necessary if a big herniated disk damages the bladder or bowel nerves. It might necessitate urgent surgery. When other therapies are unsuccessful, surgery is an option for non-emergency conditions. Although there are several approaches to spinal decompression surgery, relieving pressure on the nerve is the main objective.
Herniated Disk Prevention
Do the following to help prevent a herniated disk:
- Engage in physical exercise to strengthen the muscles of the trunk, which in turn stabilizes and supports the spine.
- Adopt a straight posture, as it reduces pressure on the spine and disks.Maintain a straight and aligned back, especially when sitting for extended periods of time. When lifting heavy objects, ensure that most of the weight is borne by the legs rather than the back.
- Maintain a healthy weight. More weight puts extra strain on the disks and spine, increasing the risk of herniation.
- Give up smoking. Don't use any tobacco products at all.
References
Mathews, H. H., & Long, B. H. (2002). Minimally invasive techniques for the treatment of intervertebral disk herniation. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 10(2), 80-85.
Milette, P. C. (2000). Classification, diagnostic imaging, and imaging characterization of a lumbar herniated disk. Radiologic Clinics, 38(6), 1267-1292.
Miwa, S., Yokogawa, A., Kobayashi, T., Nishimura, T., Igarashi, K., Inatani, H., & Tsuchiya, H. (2015). Risk factors of recurrent lumbar disk herniation. Journal of Spinal Disorders and Techniques, 28(5), E265-E269.
Modic, M. T., Masaryk, T., Boumphrey, F., Goormastic, M., & Bell, G. (1986). Lumbar herniated disk disease and canal stenosis: prospective evaluation by surface coil MR, CT, and myelography. American journal of neuroradiology, 7(4), 709-717.
Meet our doctors from the Orthopaedics department
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
Similar Posts
teleMEDCARE App
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Chronic Care
Know more about our Chronic Care Management Programme in partnership with Damana Saicohealth.

teleMEDCARE App mobile
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Spotii
We have partnered with Spotii to offer a more flexible way to pay - Pay over time for your purchase. No interest, no cost & no catch.