Written By: Dr Charles Nagy
Dr Charles Nagy is the first surgeon in the Middle East & the second globally, to be accredited & recognized by the SRC as a Master Surgeon in multidisciplinary Endometriosis care.
Updated On:May 23, 2024
Read more.

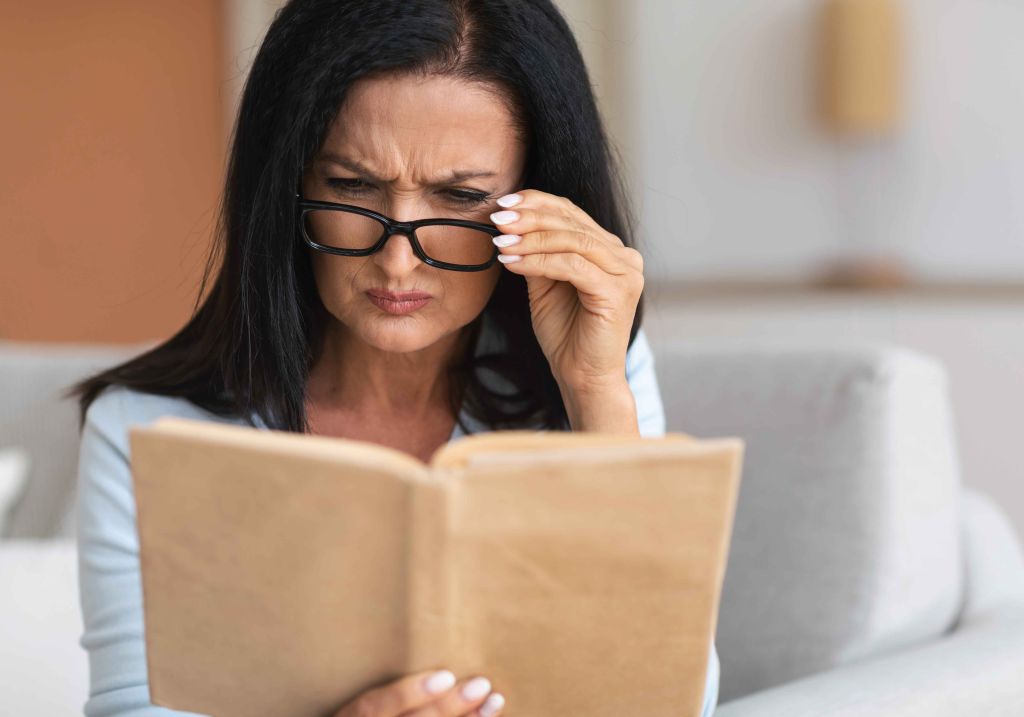
What is a Hysterectomy (Uterus Removal)?
During a hysterectomy, the uterus and the cervix are surgically removed. A hysterectomy may involve the removal of ovaries and fallopian tubes as well as surrounding organs and tissues, depending on the purpose of the operation. When a woman is pregnant, the fetus develops in the uterus. You lose blood during your menstrual cycle, which is what lines it. After a hysterectomy, you won't have your period or be able to become pregnant.
Different Types of a Hysterectomy (Uterus Removal)
Four distinct hysterectomy procedures exist:
- A total hysterectomy involves the removal of the uterus and cervix, but not the ovaries.
- Supracervical hysterectomy: Excision of only the top portion of the uterus, leaving the cervix intact.
- Removing your uterus, cervix, fallopian tubes (salpingectomy), and ovaries (oophorectomy) is known as a total hysterectomy with bilateral salpingo-oophorectomy.
- During a radical hysterectomy, your uterus, cervix, fallopian tubes, ovaries, upper vaginal region, some surrounding tissue, and lymph nodes are removed. When malignancy is present, this kind of hysterectomy is done.
Purpose of a Hysterectomy (Uterus Removal)
Medical experts perform hysterectomies to treat the following:
- Vaginal bleeding that is excessive or abnormal and cannot be addressed in any other way
- Significant menstruation discomfort that is unresponsive to medical intervention
- Benign tumors that include uterine fibroids and leiomyomas
- Uterus-related pelvic pain has gotten worse that is unresponsive to treatment
- Uterine prolapse, where the uterus "dropped" into the vaginal canal as a result of weaker support muscles, resulting in urinary incontinence or bowel obstruction
- Malignancies that have the potential to spread, including those of the uterus or the cervical area
- Conditions associated with the uterine lining include hyperplasia, recurring uterine polyps, and adenomyosis.
Procedure during a Hysterectomy (Uterus Removal)
Your healthcare professional may conduct a hysterectomy using one of numerous distinct surgical techniques, including:
Hysterectomy through vagina
- Through a cut at the top of your vagina, your uterus is removed.
- Your vagina receives dissolvable sutures.
- Most frequently applied to noncancerous (or benign) disorders like uterine prolapse.
- The favored method is regarded to have the fewest difficulties and the fastest recovery (up to four weeks).
- On the day following surgery, many patients return home.
A laparoscopic hysterectomy
- A tiny incision is made in your belly button to introduce a laparoscope, a thin tube with a video camera on the end, into your lower abdomen.
- Through several further tiny incisions, surgical instruments are introduced.
- Small incisions in the belly or a vagina can be used to remove your uterus in segments.
- Some patients leave the hospital the same day or after spending the night there.
- Compared to an abdominal hysterectomy, full recovery takes less time and hurts less.
Hysterectomy with laparoscopic robotic assistance
- The surgery is carried out by your surgeon with the aid of a robotic device.
- Your abdomen is opened up and a laparoscope is introduced to observe your pelvic region.
- Three to five small incisions are made around your belly button to introduce tiny, thin surgical instruments. The surgeon is in charge of robotic arms and equipment.
- Similar to a laparoscopic hysterectomy, the recovery is quick.
Abdominal hysterectomy
- A six to eight-inch is cut within your abdomen (either your pubic bone to your belly button or the top of your visible hairline) to remove your uterus.
- Incisions are closed by the surgeon using stitches or staples.
- Most frequently applied when uterine enlargement, malignancy, or the spread of illness to other pelvic regions are involved.
- In most cases, a lengthier hospital stay (two or three days) and a longer recuperation period are needed.
A hysterectomy takes one to three hours to perform. Your uterus's size, the need to remove scar tissue from previous procedures, and whether or not other tissues, such as endometrial tissue, and other organs (like your fallopian tubes or ovaries), are being removed at the same time as your uterus can all affect how long the procedure takes.
Benefits of Hysterectomy (Uterus Removal)
A hysterectomy can make life more pleasurable for you, especially if you experience heavy, irregular bleeding or ongoing pelvic pain. A hysterectomy might potentially reduce your chance of developing uterine cancer and save your life if you are more susceptible to the disease.
Recovery after a Hysterectomy (Uterus Removal)
Depending on the type of surgery you underwent, you may need to stay in the hospital for a different period of time after a hysterectomy. Your doctor will keep an eye on you to make sure you don't show any symptoms of problems like blood clots or bleeding. To avoid blood clots in your legs following surgery, you should start moving about right away.
If you underwent an abdominal hysterectomy, you could spend a few days in the hospital. Less invasive hysterectomies like vaginal and laparoscopic ones usually don't necessitate an overnight hospital stay.
The average recovery time following a hysterectomy is four to six weeks. Your recovery will depend on the kind of hysterectomy you underwent and how it was carried out. It takes less time to recuperate after a vaginal and laparoscopic hysterectomy than from an abdominal hysterectomy.
Gradually upping your exercise is advised, and you should also pay attention to how you feel. Stop doing anything that makes you feel uncomfortable. Your doctor will go through recuperation guidelines with you, including limitations on your regular activities. Any worries you have concerning the treatment or your recuperation should be brought up. For particular advice on how to recuperate at home, including which drugs to take, speak with your healthcare professional.
References
Carlson, K. J. (1997). Outcomes of hysterectomy. Clinical obstetrics and gynecology, 40(4), 939-946.
Carlson, K. J., Nichols, D. H., & Schiff, I. (1993). Indications for hysterectomy. New England Journal of Medicine, 328(12), 856-860.
Clarke-Pearson, D. L., & Geller, E. J. (2013). Complications of hysterectomy. Obstetrics & Gynecology, 121(3), 654-673.
Clayton, R. D. (2006). Hysterectomy. Best practice & research Clinical obstetrics & gynaecology, 20(1), 73-87.
Kjerulff, K. H., Langenberg, P. W., Rhodes, J. C., Harvey, L. A., Guzinski, G. M., & Stolley, P. D. (2000). Effectiveness of hysterectomy. Obstetrics & Gynecology, 95(3), 319-326.
Reich, H., DeCAPRIO, J. O. H. N., & McGLYNN, F. R. A. N. (1989). Laparoscopic hysterectomy. Journal of Gynecologic Surgery, 5(2), 213-216.
Soriano, D., Goldstein, A., Lecuru, F., & Darai, E. (2001). Recovery from vaginal hysterectomy compared with laparoscopy-assisted vaginal hysterectomy: a prospective, randomized, multicenter study. Acta obstetricia et gynecologica Scandinavica, 80(4), 337-337.
Meet our doctors from the Obstetrics & Gynaecology department
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
Similar Posts
teleMEDCARE App
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Chronic Care
Know more about our Chronic Care Management Programme in partnership with Damana Saicohealth.

teleMEDCARE App mobile
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Spotii
We have partnered with Spotii to offer a more flexible way to pay - Pay over time for your purchase. No interest, no cost & no catch.