Written By: Dr. Peter Nawar
Dr. Peter Nawar is a Specialist in the Department of Obstetrics & Gynaecology. After completing his basic education in Medicine, he got a Master’s Degree in Obstetrics and Gynaecology (IVF). He is a member of the American Fertility Society, the European Fertility Society, the Egyptian Association of Fertility and Sterility and the European Society of Human Reproduction and Embryology.
Updated On:January 28, 2025
Read more.

What is Miscarriage?
The unplanned termination of a pregnancy within the first 20 weeks of gestation is known as a miscarriage). The majority of miscarriages are unavoidable and happen when the fetus stops developing or is due to chromosomal abnormalities.
Causes of Miscarriage
Most first-trimester miscarriages (up to 13 weeks of pregnancy) are caused by chromosomal abnormalities. Most chromosomal issues are unintentional, and the root reason is frequently unknown. Miscarriage can also result from the following other factors:
- Infection
- Imbalances in hormones
- Improper implantation of a fertilized egg in the lining of your uterus
- Your age
- Unusual uterine conditions
- Radiation
- Thyroid condition
- Some medication
- Untreated diabetes
- Congenital heart conditions
- Severe kidney problems
- Immunological system problems
- Extreme undernutrition
The assertion that prolonged use of birth control pills, stress, physical activity, or sexual activity causes miscarriage is unsupported by any data. Regardless of your situation, it's imperative to refrain from holding yourself responsible for your loss. Most miscarriages have nothing to do with what you did or did not do.
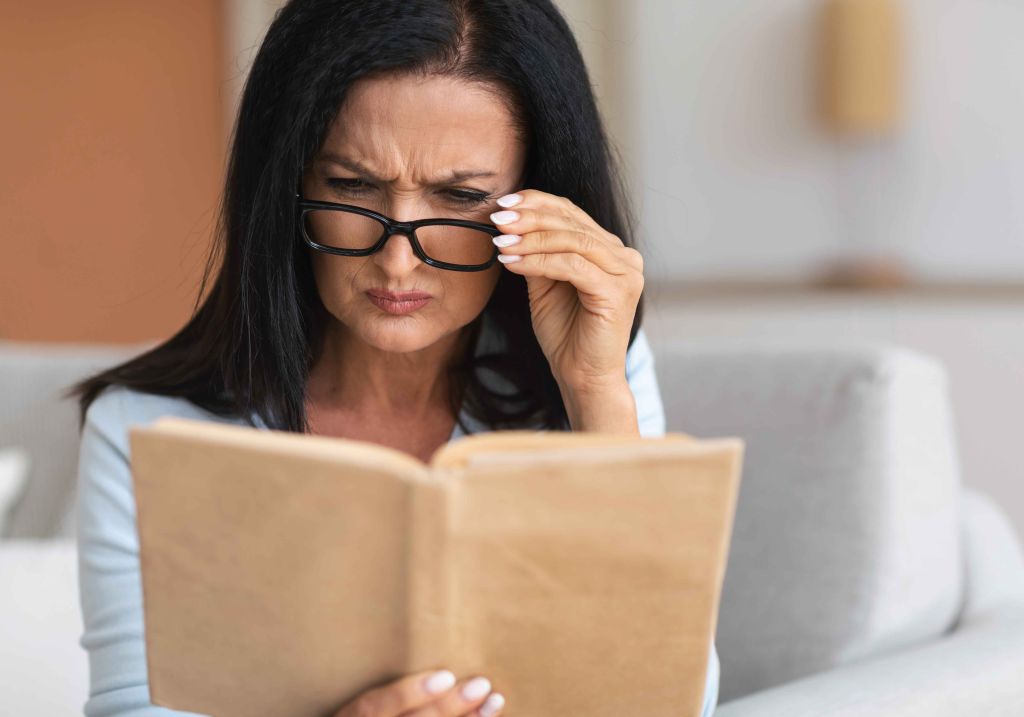
Symptoms of Miscarriage
Among the warning signs and symptoms of a miscarriage are:
- Bleeding or spotting in the vagina
- Abdominal or lower back pain or cramps
- Your vagina is leaking fluid or tissue
Place any fetal tissue you've passed from your vagina in a clean container and bring it to your doctor's office or the hospital for testing. However, it is worth mentioning that most first-trimester vaginal spotting or bleeding sufferers go on to have healthy pregnancies. Hence, spotting or bleeding may not indicate a miscarriage but consulting with your healthcare provider is a must.
When to see a doctor for Miscarriage?
If you experience intense pain and bleeding (more intense than period pain), an unusual discharge (particularly if it is foul-smelling), or fever, see a doctor or go to the emergency room at the hospital. These signs could indicate an infection or that tissue was not removed during the miscarriage.
Miscarriage Risk Factors
Miscarriage risk factors include the following:
- The chances of miscarriage increase with age.
- A chromosomal anomaly (the fetus has extra or missing chromosomes) is the primary cause of the majority of age-related miscarriages.
- Having had a previous miscarriage may potentially pose a higher risk of miscarriage.
- Having a miscarriage is more likely if you have certain medical conditions, such as uncontrolled diabetes, infections, or problems with your uterus or cervix.
- Smokers are more likely to experience a miscarriage than non-smokers.
- The use of illegal drugs and excessive alcohol both raise the risk of miscarriage.
- An increased risk of miscarriage has been associated with being overweight or underweight.
- There is a small chance of miscarriage with some invasive prenatal genetic tests, including chorionic villus collection and amniocentesis.
Miscarriage Complications
Some women who miscarry get a uterine infection. Another name for this is a septic miscarriage. The following signs can indicate a uterine infection:
- Fever and chills
- Soreness in the lower abdomen
- Bad-smelling vaginal discharge
Miscarriage Diagnosis
Your prenatal care provider will perform an ultrasound to verify a miscarriage. One of the first fetal traits your doctor can spot on an ultrasound during these examinations is the yolk sac or the fetal heartbeat. Another choice is to get a blood test for the hormone human chorionic gonadotropin (hCG), which is made by the placenta. A low hCG level can serve as confirmation of miscarriage. Last but not least, to check if your cervix has opened, your doctor could perform a pelvic exam.
A few potential diagnoses include the following:
- Threatened miscarriage: A miscarriage is possible if you are bleeding but your cervix hasn't started to dilate. These pregnancies frequently end up being successful.
- Inevitable miscarriage: A miscarriage is seen as inevitable if you are bleeding, experiencing cramps, and have a dilated cervix.
- Incomplete miscarriage: An incomplete miscarriage is when some fetus or placental material leaves your uterus after you pass it.
- Complete miscarriage: A complete miscarriage is one in which you have lost every pregnant tissue. For miscarriages that happen before 12 weeks, this is typical.
- Missed miscarriage. In a missed miscarriage, the uterus still contains placental and embryonic components, but the embryo has either already died or was never created.
- Septic miscarriage. A septic miscarriage occurs if you get an infection in your uterus. This infection may be severe, necessitating quick medical attention.
Miscarriage Treatment
Your doctor may advise sleeping until the bleeding or pain stops if a miscarriage is a threatened miscarriage. Although it hasn't been proven that bed rest can stop miscarriages, it is occasionally advised as a precaution. Exercise and sexual activity may also be prohibited. Although it hasn't been demonstrated that these actions lower the chance of miscarriage, they might make you feel more comfortable. In some circumstances, it's also a good idea to put off travel, particularly to places where it would be challenging to get prompt medical attention. If you have any forthcoming travel plans, find out from your doctor whether it would be a good idea to postpone them.
Thanks to ultrasound technology, it is now much easier to determine if an embryo died or was never developed in the event of a miscarriage. In this situation, you can have several treatment choices, which include the following:
- Expectant management. You could decide to let the miscarriage develop naturally if there are no symptoms of infection. Typically, this occurs a few weeks after it has been determined that the embryo has died. It may, regrettably, take three or four weeks. It may be emotionally challenging right now. If ejection doesn't occur naturally, you may need medical or surgical intervention.
- Medical treatment. If you'd like to expedite the procedure after learning that you've lost a particular pregnancy, medicines can help. The medication can be inserted into the vagina or administered orally. To boost the medication's effectiveness and reduce adverse effects like nausea and diarrhea, your doctor may advise vaginal administration. Within a 24-hour period, this therapy is effective for the majority of women.
- Surgical procedure. Suction dilation and curettage (D&C), a small surgical treatment, is an additional choice. Your doctor will dilate your cervix and remove tissue from the interior of your uterus during this surgery. Although complications are uncommon, they could result in harm to your cervix's connective tissue or the uterine wall. If your miscarriage is accompanied by significant bleeding or symptoms of an infection, surgery may be necessary.
Miscarriage Prevention
A miscarriage typically cannot be stopped. If you miscarry, it is not your fault. The best thing you can do while pregnant is to take good care of your body. Here are a few illustrations of self-care techniques:
- Showing up for all of your prenatal visits.
- Retaining a healthy weight
- Refraining from smoking and/or drinking
- Taking prenatal vitamins
- Eating healthfully and working out frequently
References
Elina Hemminki, M. D. (1998). Treatment of miscarriage: current practice and rationale. Obstetrics & Gynecology, 91(2), 247-253.
Giakoumelou, S., Wheelhouse, N., Cuschieri, K., Entrican, G., Howie, S. E., & Horne, A. W. (2016). The role of infection in miscarriage. Human reproduction update, 22(1), 116-133.
Jeve, Y. B., & Davies, W. (2014). Evidence-based management of recurrent miscarriages. Journal of human reproductive sciences, 7(3), 159.
Neilson, J. P., Gyte, G. M., Hickey, M., Vazquez, J. C., & Dou, L. (2013). Medical treatments for incomplete miscarriage. Cochrane Database of Systematic Reviews, (3).
Sharma, B., Deep, J., Pandit, C., Basnyat, B., Khanal, B., Raut, B. B., ... & Basyal, R. (2020). Overview on current approach on recurrent miscarriage and threatened miscarriage. Clin J Obstet Gynecol, 3, 151-157.
Meet our doctors from the Obstetrics & Gynaecology department
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
|
||||||||
Similar Posts
teleMEDCARE App
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Chronic Care
Know more about our Chronic Care Management Programme in partnership with Damana Saicohealth.

teleMEDCARE App mobile
Download teleMEDCARE app from Google Play or App Store to connect immediately to Medcare doctors at a click of a button and without an appointment.

Home Services
We offer our patients a broad range of home health care services in the comfort of their own homes. Book an appointment for lab tests, vaccinations, nurses and physiotherapists.

Spotii
We have partnered with Spotii to offer a more flexible way to pay - Pay over time for your purchase. No interest, no cost & no catch.